We asked Esme Foxworthy-Bowers, our Facilitator in Scotland, to reflect on 2022. Esme’s Facilitator is in Glasgow, and aims to increase the use of technology in care at home services. She is reviewing and synthesising evidence to support the implementation of a new model developed by Scottish Care.
IMPACT Facilitators work within a local organisation, leading an evidence-informed change project. Through close collaboration, facilitators review the evidence, lead local change and evaluate the effectiveness of the changes that take place. In order to encourage replication across the social care sector, we will share our successful findings and outcomes with others.
What have been your highlights of 2022?
I’ve been working with Baillieston Community Care in Glasgow on technology implementation, with their care at home services. This is working alongside the Scottish Care project of ‘Care Technologists’. The role supports people to access care and helps them use technology as part of their everyday activities. To understand what has been working well or needs improvement, I’ve spoken to some of the people that the Baillieston Care Technologist has been working with. This has been one of my highlights. It has been great to be on the ground as staff and people who use the care-at-home service have learned more about technology.
Working with the Care Technologists has been another highlight for me. The team is so enthusiastic and has been doing fantastic information sharing with me! The project is allowing people who use care-at-home services and staff who provide support to identify the changes they would like to see, and to express their thoughts and opinions.
The number of opportunities for learning during this project has really impressed me. Scotland is currently working to develop a National Care Service. I’ve been in meetings where I have spoken about IMPACT’s work and the Facilitator project with individuals from the National Care Service working groups. The results will help them incorporate the practice knowledge and lived experience evidence into the development of the National Care Service. It would be incredible to see the work from this project used for such a large-scale re-design of care at home.
What have been the challenges this year?
At the beginning of my role, it was difficult to find information about previous technology projects or tests of change in the care at home sector. This prevented me from getting a grasp of what was already being done. I also needed to find out more about technology implementation. Initially, this was harder than I anticipated to navigate. A big part of my job is around evidence-based information ‘brokering’, and there isn’t a lot of information available or published at present.
How have your aspirations for the project/IMPACT changed?
I think now that the groundwork with Baillieston Community Care has been laid, my aspirations have shifted more toward plans for the Facilitator project itself. Personally, I love the information distribution aspect of this job. I want Baillieston Community Care to feel like they have more options, more knowledge, and are more enabled to explore technology in their service by the end of the pilot.
What have you learned so far?
So far, the gap between practice and research has been particularly emphasised. There is not a lot of large-scale research on technology in care at home, and services are often very stretched due to staff shortages and time.
A learning point for me was really emphasised by the equality, diversity and inclusion training that IMPACT staff attended in November 2022. This really highlighted the need for everyone in the system not to be viewed as cogs in a machine. I realised that everyone in a service has their own worries, lives, hopes and happiness to think about every day. I think this notion is consistent with the way that carers and people accessing care view technology. There is not one size that fits all and it is very individual. There is also a real worry that staff will be replaced by technology. Often this worry overshadows the potential for technology to complement care and support.
What are your hopes for next year?
I will be engaging more staff at Baillieston about IMPACT and the Facilitator project. I will also find out what kinds of technology would make a real difference. Through this, I hope I can bring an understanding of the background evidence for using technology in care at home in a way that acknowledges but takes steps to remove the fear that is sometimes present.
I am hopeful that this project can allow staff to work in ways that suit the needs of their role. They will begin to work with technology that’s suited to both them and the people accessing care. I hope the Facilitator project allows multiple organisations to understand their staff and the people that access care. Ultimately, enabling them to design ways of working that suit everyone.
What does success look like?
Success for me is ensuring that Baillieston’s hopes for this project are fulfilled. Baillieston Community Care is hoping to increase staff confidence with technology. They also want to develop case studies that can demonstrate what helps and hinders the use of technology in care at home services. This might identify the need for training in digital skills for example. By working with the Care Technologists this may encourage questions to them, which might alleviate some concerns or difficulties people face which they’re unsure about how to solve.
Conversely, it’s also becoming clear that part of success in a technological context is recognising hesitancy when using technology. Whilst there are benefits to assistive technology and information provision, digital access is about maintaining the right of people to say no to technology. Success in this context means that people benefit from technology if they choose it, and staff feels able to implement and use technology in care at home.
I think importantly, this success comes from the Facilitator contributing to evidence-based practice in this way. I am effectively distributing and encouraging the use of evidence-based practice.
What’s unique about your ‘technology in care’ project?
It’s become clear from my work so far that it is easy to assume that many social care organisations already have technology and technological skills. However, this is not necessarily the case. My hope is that confidence will increase in the future. To do this, I think we need to understand the needs, wants and fears of technology from staff and people accessing care at home.
I feel that there is a real opportunity for the Facilitator project to support this. In the future, I hope we will be able to help people in geographically different areas using technology (especially as social care provision can look very different in remote and rural areas).
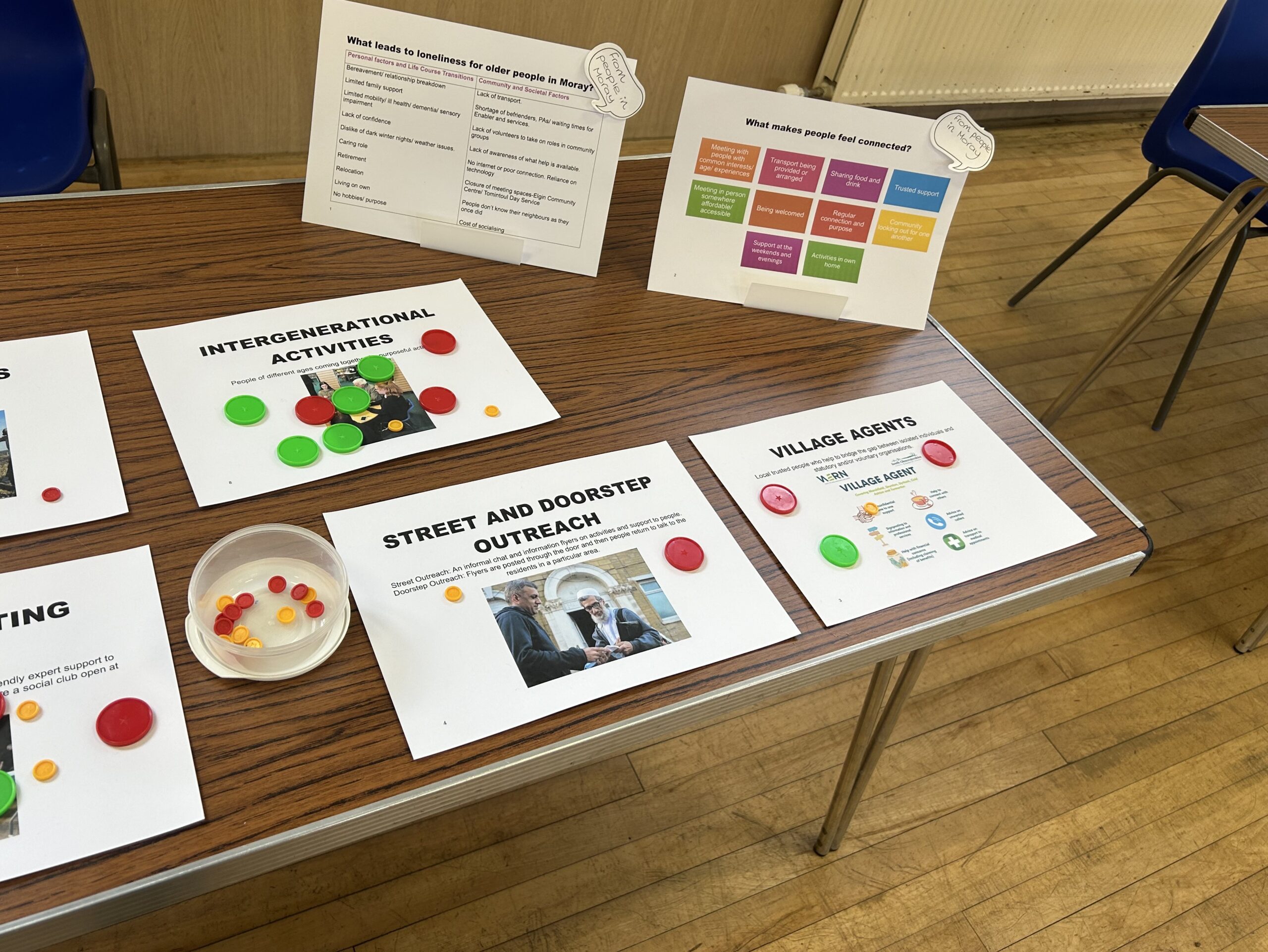
A real surprise for me has been running focus groups. There have been some productive discussions about what is working and not working in terms of technology and implementation. There have also been success stories and practical knowledge sharing.
I also feel I’ve become a better ‘knowledge broker’. It has been great to experience people coming to me to ask if can share any research relating to technology implementation. This part of the Facilitator role has slotted very well into the social care setting and it feels as if I am providing a useful and relevant role. It is also great learning for the Facilitators of the future after the pilot year!